By Dr Sam Bendall and Dr Bethan Richards

Dr Sam Bendall 
Dr Bethan Richards
1. What do you think are the top 3 reasons to focus on staff wellbeing in our EDs and Health Services?
1. Firstly, Safety – for staff and patients.
From day one in medical school, we are taught that patients must always come first – no matter what. This doctrine is firmly reinforced throughout our medical careers. For most doctors, it is accompanied by a sense of both duty and pride.
What we have come to realise in modern day medicine is that this rigid approach is completely unsustainable and has led to an epidemic of clinician burnout. A vast body of literature shows that burnout is bad for the individual and for patient care. Clinicians suffering from burnout have higher rates of absenteeism, drug and alcohol abuse, relationship breakdown, depression, anxiety and suicide. From a quality and safety perspective, burnout is also associated with an increase in medical errors, reduced patient satisfaction, and reduced quality of care.
Focussing on staff wellbeing is therefore critical if we are to meaningfully address the burnout epidemic and its tragic consequences for clinicians and our patients. If we put people first, not just patients first, we all do better.
2. The second reason to focus on staff wellbeing is to create environments where clinicians can be at their best
Investing in wellbeing is not just about encouraging staff to take care of themselves. It is about creating an environment – physical, psychological and social, where clinicians as humans can thrive and perform at their best (and not just at work!).
In addition to having their basic needs met, humans need to feel physically and psychologically safe. Connected, valued and that they belong to a group, in order to thrive. Emergency Departments and Health Services are demanding and physically, mentally and emotionally challenging workplaces. Focussing on wellbeing doesn’t mean just addressing our basic needs. It also means focussing on effective leadership and the creation and perpetuation of a culture that creates an environment where it is safe to speak up, input is valued, and people feel appreciated for what they bring to the team. When people feel psychologically safe, they will speak up and identify safety risks, collaborate better, come forward with innovative ideas and tend to stay in a workplace longer with less absenteeism.
I work half time in ED and half time in Aeromedical retrieval. They are very different cultures. Aeromedical retrieval has a very strong focus on excellence in leadership and human factors, for the safety of our teams and our patients. By making our psychological environment safe to speak up, we lower the chance of putting our patients, our teams and ourselves at risk. In order to do that, we train every six months in human factors and non-technical skills to ensure that everyone has the same knowledge and is skilled at using it. Our safety reporting is also a no-blame system with a Safety II focus which helps us all learn when things go wrong. There is also a very strong emphasis on mitigating the psychological impact of what we do, as we are one of the highest risk groups for posttraumatic stress disorder PTSD. NSW Ambulance has a “risk register” for those involved in emotionally challenging jobs and they are followed up by friends and wellbeing leads. A clinical psychologist is present on base and the chaplains visit regularly. Every job is debriefed openly. This all helps to maintain psychological and emotional wellbeing in a high-risk group. I would love to see this same framework, training and rigour applied in Emergency Departments and Hospitals to create cultures and environments where clinicians can be at their best. It works.
Psychological safety is a belief that one will not be punished or humiliated for speaking up with ideas, questions, concerns or mistakes”
(Professor Amy Edmondson)
Building a psychologically safe workplace – Professor Amy Edmondson (Novartis professor of Leadership and Management, Harvard Business School)
3. Thirdly, ED’s and Health services focussing on wellbeing enhances Clinician Engagement
Clinicians suffering from burnout are much less likely to engage constructively with the department and organisation and be positive in their interactions with patients and other staff. A high level of clinician engagement is integral to the effective function of a safe and successful department and organisation. Employee engagement is also a measure of success for administrators, so it is a win-win to aim for.

By addressing the variety of drivers of burnout and creating a Culture of Wellness where clinicians feel valued and professionally fulfilled, clinician engagement will improve. Over time this will build social capital which is the goodwill, trust and interconnectedness available to organisations that accrues from the capability of employees to work together for common purposes.1 Organisations that have a high level of social capital by nature have high levels of employee engagement and are conducive to the formation and function of high performing teams.
2. What are your top 3 tips for the clinician who is thinking about bringing a wellbeing optimisation proposal (business case) to their hospital executive (to optimise buy in and subsequent financial support)?
1. Sell the Why.
Don’t assume that audience will know this. Hospital executives are human beings and the case for addressing burnout is incredibly strong. Explain what burnout is, why it is important and what the tragic impacts of it are to the individual, to the organisation and to patient care. Ensure your message is clear that addressing burnout is a shared responsibility between the organisation and the individual, with the majority of drivers being at an organisational level. Tell a story – an emotional connection will always be a more powerful sell.


Shanafelt,TD, Noseworthy, JH: :Mayo Clin Proc January 2017;92(1):129-146 n http://dx.doi.org/10.1016/j.mayocp.2016.10.004
2. Local data is powerful
Whilst presenting statistics from the literature is useful, having local data to support your business case will be far more powerful. Measure your staff burnout rates and benchmark them against international comparators. Look at KPIs that are important to your administration. In NSW that could be the People Matters Survey, clinician engagement etc. Look at your baseline error rates and what these might cost. Don’t reinvent the wheel, talk to colleagues and review their business cases (i.e MDOK 😊)

3. Find an Executive Sponsor
Do your research, start small and look for quick wins. Find an executive sponsor who will back your proposal. Don’t reinvent the wheel. Look at what has worked (Stanford WellMD, MDOK). Focus on achievable goals so as not to overwhelm exec and not set yourself up for failure.


3. What do you mean when you say the missing KPI is Physician Wellness?
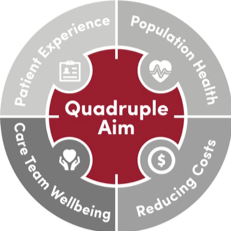
The Institute for Healthcare Improvement (IHI)Triple aim is a framework to describe an approach to optimising health system performance. The Triple aim states that in order to do that, three domains must be pursued simultaneously. These are:
1. Improving the patient experience of care (including quality and satisfaction)
2. Improving the health of populations and
3. Reducing the per capita cost of health care,
However, the missing piece of the puzzle here is clinician wellness. Without taking care of our staff and creating an environment where they can feel valued, professionally fulfilled and psychologically safe, we are unlikely to achieve any of the first three effectively. Improved patient care, lower costs and better outcomes are all contingent on clinicians being well and able to be at their best. This is the fourth KPI – clinician wellbeing.
https://uofuhealth.utah.edu/notes/postings/2019/10/strategy-wellbeing.php
4. Finally, attending the Chief Wellness Officer Course at Stanford Well MD centre, is a dream for many involved in promoting change in the area of wellness at work. What are the top 2 concepts from Well MD that you felt helped your own projects here in NSW?
1. Effective Leadership is an absolute cornerstone
This was one of my biggest lessons from the course. Effective leadership is a key driver of wellbeing for clinicians however few clinicians have ever had any formal training on how to lead and few organisations grow their own leaders. Those who do (e.g. the Mayo Clinic) reap the rewards. Improving the leadership skills and styles of senior leaders has a direct effect on wellbeing for those under their care.
As Simon Sinek says, leadership is not being in charge, it is about taking care of those in your charge.

2. Don’t boil the ocean
When you are starting a wellbeing program, start small and focus on where the evidence lies. Get some runs on the board and build deliberately. If you try and spread yourself or your resources too thinly you won’t succeed. Small, planned and gradual successes are better and build faith in your program. This is why we started MDOK for doctors as that is where the evidence lies but the aim is to broaden this to all staff, and we are already on that journey which is great to see.

References
1. Swensen,S, Gorringe G: Leadership by Design: Intentional Organization Development of Physician Leaders Journal of Management Development Vol. 35 No. 4, 2016 pp. 549-570
2. Shanafelt,TD, Noseworthy, JH: Mayo Clin Proc January 2017;92(1):129-146 n http://dx.doi.org/10.1016/j.mayocp.2016.10.004
Did you know @wrapemtweet has a complete clinician developed, peer reviewed, easy to use wellbeing curriculum for you to use, any time you like. Check out https://wrapem.org/modules/modules-user-guide/

